Osteoporosis is often considered a silent disease because bone damage occurs silently, without early pain or obvious warning signs. Many people feel healthy for years while their bones gradually lose strength, making them brittle and prone to fracture. by the time osteoporosis symptoms appear, the loss of bone density may already be severe enough to affect daily life and mobility.
This condition affects millions of people around the world, especially women after menopause and older adults. As bone tissue breaks down faster than it is rebuilt, the skeletal structure becomes weaker and less resilient. Understanding how osteoporosis develops, what signs to look out for, and how it can be detected early is essential to protecting long-term bone health and independence.
Osteoporosis symptoms and early warning signs
Osteoporosis symptoms tend to appear only after significant weakening of the bones has occurred. Common signs include a gradual loss of height, a hunched posture caused by compression fractures of the spine, and persistent back pain that develops without a clear injury. Fractures of the hip, wrist, or spine from minor falls or simple movements often indicate advanced loss of bone density.
According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), many people with osteoporosis do not experience symptoms until a fracture occurs, which is why screening is strongly recommended for high-risk individuals. The agency explains that spinal fractures can occur silently, contributing to postural changes and reduced mobility over time.
Because the symptoms are subtle, osteoporosis is often overlooked. Paying attention to physical changes and risk factors helps prompt earlier testing before serious fractures develop.
Causes and risk factors behind bone density loss
Bone density loss occurs when the body breaks down bone tissue faster than it can rebuild it. Hormonal changes play an important role, particularly the drop in estrogen after menopause, which accelerates bone resorption. In men, lower testosterone levels with age also contribute to gradual thinning of bones.
Based on information from the US Office of the Surgeon GeneralLifestyle factors such as low calcium intake, vitamin D deficiency, smoking and excessive alcohol consumption significantly increase the risk of osteoporosis. Long-term use of corticosteroids and certain medical conditions, including thyroid disorders and autoimmune diseases, further impair bone remodeling.
Genetics also influences maximum bone mass and long-term bone strength. When multiple risk factors combine, bone density loss can rapidly accelerate, increasing the risk of fracture even in relatively active people.
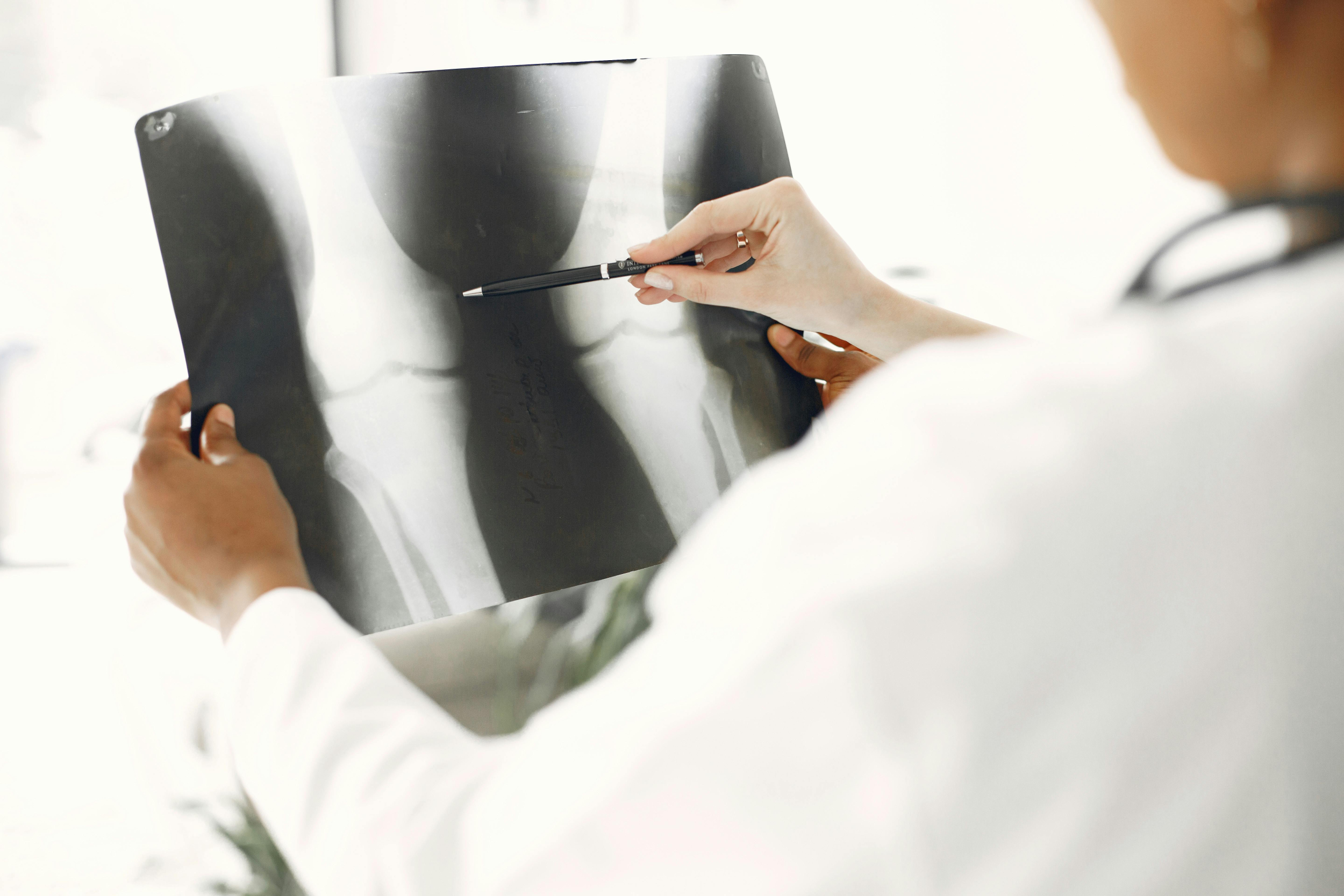
How osteoporosis is diagnosed early
Diagnosing osteoporosis before fractures occur is based on imaging and risk assessment rather than physical symptoms alone. The main diagnostic tool is a DXA scan, which measures bone mineral density in the hip and spine. A T score of -2.5 or lower confirms osteoporosis, while scores between -1.0 and -2.5 indicate low bone mass.
According to the International Osteoporosis FoundationDXA scanning is the most reliable method for identifying fracture risk and monitoring bone changes over time. The organization also highlights fracture risk calculators, such as FRAX, which estimate the probability that a person will suffer a fracture within ten years.
Early diagnosis allows treatment to begin before irreversible bone damage occurs, reducing the likelihood of life-altering fractures.
Prevention and treatment options that protect bone health
Preventing osteoporosis focuses on slowing the loss of bone density and strengthening existing bone. Weight-bearing activities, such as walking, stair climbing, and resistance training, stimulate bone formation and improve balance. Adequate intake of calcium and vitamin D promotes mineralization and helps maintain bone structure.
Treatment options include medications that slow bone breakdown or stimulate new bone growth. Bisphosphonates reduce the risk of fractures by limiting osteoclast activity, while newer therapies stimulate bone formation in severe cases. Lifestyle changes, fall prevention strategies, and regular monitoring work together to preserve mobility and independence as people age.
Build stronger bones for a safer future
Protecting bone health requires awareness long before osteoporosis symptoms appear. When bone density loss is identified early, specific changes in lifestyle and medical care can dramatically reduce the risk of fractures. Strong bones promote mobility, confidence and quality of life well into old age.
By understanding risk factors, prioritizing screening, and committing to consistent prevention habits, people can stay active and resilient. Bone health isn’t just about avoiding fractures: it’s about maintaining long-term freedom of movement and independence for years to come.
Frequently asked questions
1. What are the first symptoms of osteoporosis to pay attention to?
The first symptoms of osteoporosis are usually subtle or completely absent. Some people notice a gradual loss of height or mild back discomfort over time. Because pain is uncommon from the beginning, fractures may be the first noticeable sign. That’s why it’s important to get screened even without symptoms.
2. Can bone density loss be reversed?
Severe bone density loss is difficult to completely reverse, but can often be slowed or partially improved. Medications, proper nutrition, and weight-bearing exercise help strengthen bones. Early intervention produces the best results. Ongoing monitoring helps guide treatment adjustments.
3. Who should be tested for osteoporosis?
It is generally recommended that women over 65 and men over 70 get tested. Younger people with risk factors such as early menopause, steroid use, or family history may need earlier screening. Doctors may recommend testing after fractures from minor falls. Personalized risk assessment guides timing.
4. Is osteoporosis only a concern for women?
While osteoporosis is more common in women, men are also affected. Men tend to develop it later in life, but face higher mortality after a hip fracture. Hormonal changes, lifestyle factors, and medical conditions contribute to risk in both sexes. Awareness and prevention are important for everyone.