Psoriasis is often considered a superficial problem, but red, scaly plaques on the skin can be a visible sign of a deeper problem. inflammatory process. As understanding of this autoimmune skin condition has increased, researchers now recognize that psoriasis symptoms may reflect widespread immune activity that affects joints, blood vessels, and metabolism.
Viewing psoriasis through this systemic lens can change the way people think about diagnosis, treatment, and long-term health.
Understanding psoriasis as an autoimmune skin condition
Describing psoriasis as an autoimmune skin condition highlights the role of the immune system in driving the disease.
In autoimmune and immune-mediated diseases, the body’s defenses are bypassed, causing chronic inflammation even in the absence of infection. In psoriasis, this inflammation is centered on the skin and, in some people, the joints.
Some experts refer to psoriasis as autoimmune and autoinflammatory because it involves elements of classical autoimmunity and innate immune activation.
Regardless of the terminology, the key idea is that psoriasis is not caused by poor hygiene or simple irritation. It is a biologically complex condition with genetic and environmental contributors, and its symptoms reflect immune pathways that can also affect other organs.
Recognize the common symptoms of psoriasis
Psoriasis symptoms It may look different from person to person, but there are several traits that are particularly characteristic. The most common form, plaque psoriasis, usually presents with:
Raised, thickened patches of skin covered with silvery-white or grayish scales. Red, pink or purple discoloration, depending on skin tone. Injuries most commonly found on the elbows, knees, scalp, and lower back.
Many people report itching, burning, or pain in the affected areas, which can interfere with sleep and daily activities. The skin may become dry and cracked, with occasional bleeding when the plaques are irritated or scratched. The scalp may have intense flaking that resembles severe dandruff.
The symptoms of psoriasis are not limited to the skin. Nail changes are common, including pitting (small depressions), ridges, discoloration, and separation of the nail from the nail bed.
Different subtypes, such as guttate, pustular, inverse, and erythrodermic psoriasis, have their own symptom patterns, ranging from small, droplet-like spots to widespread redness or pus-filled bumps. This diversity is one of the reasons why a professional evaluation is important when symptoms first appear.
How psoriasis is connected to systemic inflammation
The connection between psoriasis and systemic inflammation lies in immune pathways that cause skin lesions and deeper health effects. Immune cells in psoriatic plaques produce cytokines, chemical messengers that promote inflammation.
These cytokines do not remain confined to the skin; They circulate in the bloodstream and potentially affect the lining of blood vessels, joints and other tissues, according to Mayo Clinic.
This knowledge supports the view of psoriasis as part of a broader inflammatory network that can increase the risk of other conditions. In this sense, psoriasis symptoms on the skin can serve as a visible marker of underlying immune activity that may be silently occurring elsewhere in the body.
Recognizing this connection has encouraged more comprehensive care, paying attention not only to skin cleansing but also to overall inflammatory burden.
Triggers that worsen psoriasis symptoms and inflammation
Psoriasis symptoms often fluctuate over time, with periods of relative calm and sudden flare-ups. A variety of triggers can worsen the condition, including:
Infections, particularly strep throat infections in guttate psoriasis Skin injuries such as cuts, scrapes, or sunburn (Koebner’s phenomenon) Psychological stress and lack of sleep Certain medications, including some blood pressure medications and antimalarials Smoking and heavy alcohol use
Lifestyle factors also play an important role. Obesity and inactivity can promote systemic inflammation and increase disease severity. Dietary patterns high in processed foods and low in fruits, vegetables, and whole grains may contribute to an inflammatory state.
Genetics and family history further influence who develops psoriasis and its severity, highlighting the interplay between inherited risk and environmental exposures.
Diagnosis and evaluation of systemic involvement
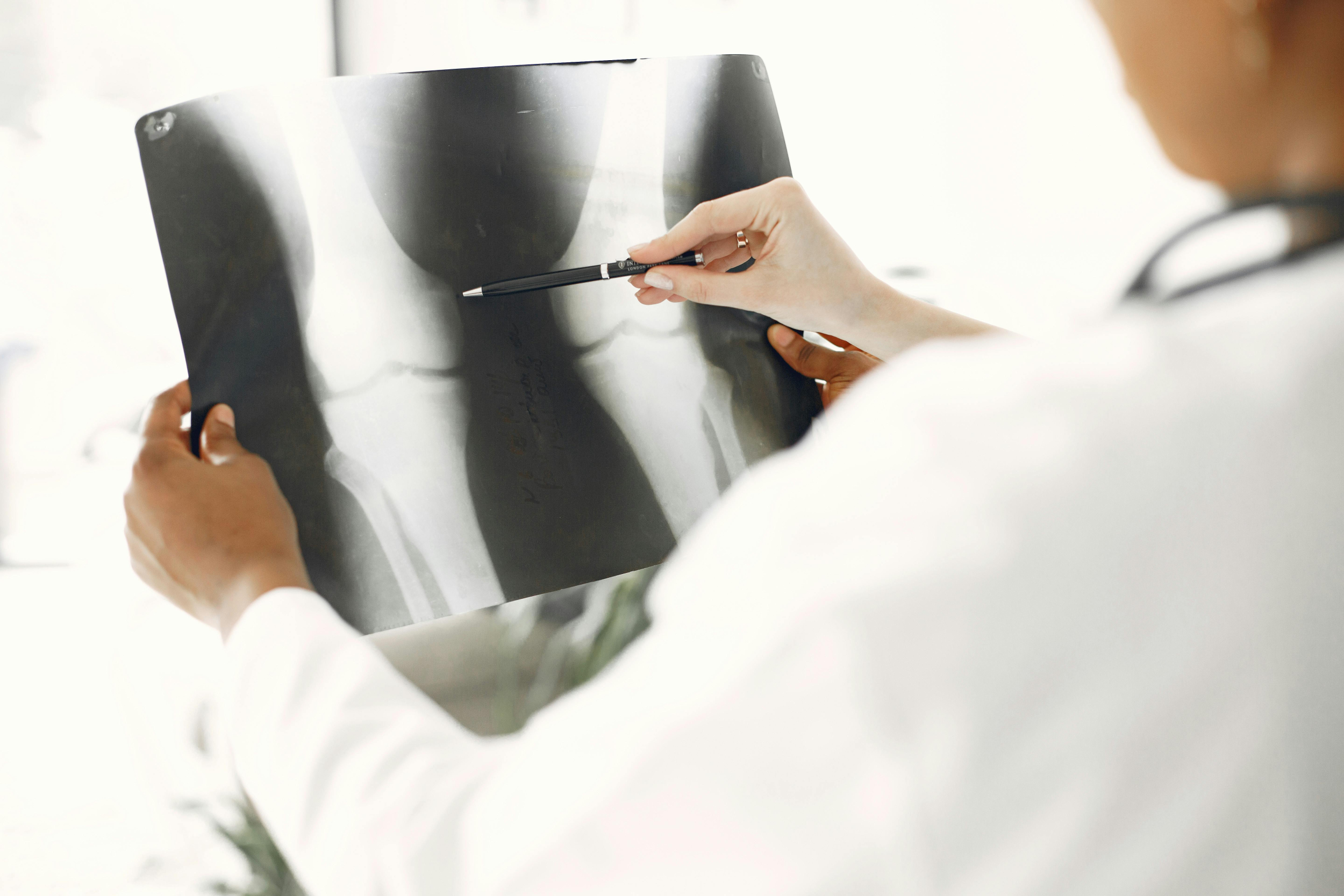
The diagnosis of psoriasis is usually clinical, based on the appearance and distribution of the lesions and the presence of characteristic scaling.
Dermatologists may perform a skin biopsy in uncertain cases to confirm the diagnosis and rule out other conditions. Because psoriasis is related to systemic inflammation, many experts also recommend screening for comorbidities.
A thorough evaluation may include questions about joint pain, stiffness, and swelling to identify psoriatic arthritis. Blood pressure, weight, waist circumference, and basic blood tests can help assess cardiovascular and metabolic risk.
In some cases, referral to rheumatology or other specialists is appropriate. Addressing psoriasis in this integrated way supports early detection of related conditions and more comprehensive treatment.
Treatment Options for Skin and Systemic Inflammation
Treatment strategies for psoriasis aim to relieve symptoms, improve the appearance and function of the skin, and reduce underlying inflammatory activity. For mild disease, topical therapies are usually the first option.
These include creams and ointments with corticosteroids, vitamin D analogs, retinoids, calcineurin inhibitors, and other medicinal products that reduce inflammation and slow the growth of skin cells, according to Cleveland Clinic.
For more extensive or resistant psoriasis, phototherapy (controlled exposure to ultraviolet light) may be effective. Systemic medications such as methotrexate, cyclosporine, and newer oral agents are used to modulate immune responses in moderate to severe cases.
Biological therapies have become an important advance; These drugs target specific molecules such as interleukin-17, interleukin-23, or tumor necrosis factor alpha. By targeting key inflammatory pathways, biologics can improve both skin and joint symptoms and may help reduce overall inflammatory burden.
The choice of treatment depends on the severity of the disease, comorbid conditions, patient preferences, and safety considerations. Regular monitoring is important to monitor effectiveness, side effects, and long-term health.
Psoriasis Symptoms as a Clue to Whole Body Health
When psoriasis is considered only a cosmetic concern, opportunities to protect long-term health may be missed. Recognizing it as an autoimmune skin condition that reflects broader immune activity changes the conversation.
Skin lesions, nail changes, and joint symptoms can act as visible clues to underlying systemic inflammation, providing an early opportunity to identify and address associated risks.
People living with psoriasis benefit from collaborative care that includes dermatology, primary care, and, when appropriate, rheumatology or cardiology. Open communication about new or changing symptoms, treatment goals, and lifestyle challenges helps design a plan that addresses both the skin and the whole person.
By integrating medical therapy By paying attention to cardiovascular, metabolic, and joint health, psoriasis can be treated not only as a skin disease but as a key window to overall inflammatory wellness.
Frequently asked questions
1. Can someone have psoriasis without the classic red, scaly plaques?
Yes. Psoriasis can appear as soft red spots in the folds of the skin, affect only the nails, or show primarily as joint pain with minimal visible skin changes.
2. If psoriasis is an autoimmune skin condition, does that mean the immune system is “weak”?
No. The immune system is overactive and misdirected, creating chronic inflammation, not too weak to fight infections.
3. Can psoriasis go into remission and what does that look like?
Yes. The plaques may flatten or disappear, the itching may disappear, and the skin may look almost normal, although breakouts may return.
4. How is psoriasis different from eczema if both cause itchy and inflamed skin?
Psoriasis usually forms thick, scaly, sharp-edged plaques and is strongly linked to systemic inflammation; Eczema tends to be less defined, may ooze, and is more related to allergies and a weak skin barrier.