The National Institutes of Health awarded a five-year, $2.8 million grant to researchers at UTHealth Houston to evaluate long-term effects on patients enrolled in the “Cryopreserved Human Umbilical Cord as a Meningeal Patch in Fetoscopic Spina Bifida Repair” trial.
The study is led by Ramesha Papanna, MD, MPH, a professor at UTHealth Houston McGovern Medical School and a maternal-fetal surgeon at UTHealth Houston Fetal Center and Children’s Memorial Hermann Hospital.
The funding will allow patients enrolled in the first-of-its-kind fetoscopic spina bifida repair study to be monitored until they are 30 months old.
The investigators will analyze neurological, motor, and developmental outcomes and their correlation with radiological markers of spinal cord tethering in patients who took part in the study.
“It is remarkable that an idea we had 13 years ago has become a therapy that improves outcomes for children with spina bifida, helping them walk faster,” said Papanna, internationally recognized for his research on improving outcomes after fetal intervention and research into methods for preventing preterm birth. “Advancing from bench concept to FDA Phase 3 trial, supported by NIH grants, has been extraordinary. This new funding for the efficacy trial, which already shows improvements in mobility, highlights the impact and promise for patients.”
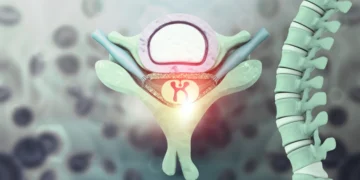
Spina bifida affects approximately 1 in 2,875 births in the U.S. each year. Neural tube defect occurs when the spine and spinal cord do not close properly during the early stages of pregnancy, causing varying degrees of disability, such as leg weakness, paralysis, and bladder or bowel problems. The condition can be classified into three levels of severity: spina bifida occulta (mild), meningocele (moderate), and myelomeningocele (severe).
While there is no cure, treatment for the condition includes surgery, ongoing medical care, and physical therapy.
The UTHealth Houston team is currently in the final stage of testing the trial after successfully completing an early feasibility trial to establish the safety of the procedure.
Patients enrolled in the trial undergo a fetoscopic procedure that differs from open in-utero repair, which requires a large incision in the uterus and delivery by cesarean section. Instead, the fetal intervention team repairs the spina bifida defect in two layers through three small incisions in the uterus using a fetoscope, a high-resolution camera, and small surgical instruments. The first layer is closed using a cryopreserved human umbilical cord patch placed over the spinal cord, followed by a second layer of primary skin closure. Mothers have vaginal delivery, unless there is an obstetric indication for a cesarean section.
Once delivered, a team of experts, who are co-investigators on the trial, schedule appointments for follow-up evaluations at 12 and 30 months.
The team includes Stephen Fletcher, DO, Dr. Marnie Rose Professor of Pediatric Neurosurgery at McGovern Medical School and pediatric neurosurgeon at the UTHealth Houston Fetal Center; Gabriel Anzueto, MD, Raghuthaman Family Professor in Pediatric Neurology and Developmental-Behavioral Pediatrics at McGovern Medical School and developmental pediatrician at UT Physicians; and Rajan Patel, MD, pediatric neuroradiologist at Texas Children’s Hospital.
During these appointments, children undergo comprehensive neurological and developmental evaluations, as well as MRIs of the brain and spinal cord.
Follow-up is essential, not only for the care of each child but also for the success of the study. “These assessments show us how children are progressing after this innovative therapy and help identify both positive outcomes and areas that may need attention.”
Ramesha Papanna, MD, MPH, professor, UTHealth Houston McGovern School of Medicine
Other UTHealth Houston clinical collaborators for the study include McGovern Medical School and Fetal Center’s KuoJen Tsao, MD, The Children’s Fund, Inc. Distinguished Professor of Pediatric Surgery and pediatric general and thoracic surgeon; Jimmy Espinoza, MD, professor of obstetrics, gynecology and reproductive sciences and obstetrician-gynecologist; Sami Backley, MD, assistant professor of obstetrics, gynecology and reproductive sciences and maternal-fetal medicine specialist; Peter Yang, MD, assistant professor of pediatric neurosurgery and pediatric neurosurgeon; Jason Au, MD, assistant professor of diagnostic and interventional imaging and pediatric urologist; and Suzanne López, MD, professor of neonatal-perinatal medicine and neonatologist. Research collaborators involved in the trial include Lovepreet K. Mann, MBBS, associate professor of obstetrics, gynecology and reproductive sciences, and Dejian Lai, PhD, professor of biostatics at the UTHealth Houston School of Public Health.
Families and physicians looking for more information about how to enroll in the trial can visit the UTHealth Houston Fetal Center trial page.