New evidence urges attention to TMP-SMX antibiotics in early pregnancy, highlighting safer options for treating urinary tract infections.
Study: Use of early pregnancy antibiotics for the risk of urinary tract infections and congenital malformations. Image credit: Henadzipechan / Shutterstock
In a recent study published in JAMA Network Open, researchers assessed the risk of congenital malformations following antibiotic treatment for first-stage pregnancy urinary tract infection (UTI).
UTIs such as acute cystitis and asymptomatic bacteriuria (ASB) are common in pregnancy and are associated with adverse outcomes including low birth weight, premature birth, maternal sepsis, and nephrone nephritis. The first prenatal visit recommends routine ASB screening, often leading to antibiotic therapy in the early stages of pregnancy.
However, studies have raised concerns about the higher risk of congenital malformations associated with two antibiotics used in UTI treatments: trimethoprim-sulfamethoxazole (TMP-SMX) and nitrofurantoin, which have significant methodological limitations to these studies. Therefore, evidence regarding the safety of antibiotics during pregnancy is necessary to guide clinical practice.
About the research
In this study, the researchers investigated whether TMP-SMX, fluoroquinolone, and nitrofluntine are associated with congenital malformations compared to other antibiotics used in UTI treatments in the United States (USA). First, mid-term pregnancy and birth infants were administered UTI antibiotics, and identified from a commercially insured population between 2006 and 2022.
Individuals receiving multiple UTI-related antibiotics, as well as pregnant women exposed to spinal cord injuries, immunosuppression, chromosomal abnormalities, and early pregnancy teratogenic drugs were excluded. The outpatient pharmacy claims were used to identify antibiotics distributed for UTI treatments, including TMP-SMX, nitrophantin, β-lactam, and fluoroquinolone (ofloxacin, ciprofloxacin, levofloxacin).
Beta-lactams were used as reference as these agents were considered safe during pregnancy. The results of this study were Kharbanda et al. The logarithmic regression model assessed the association between antibiotics and risk of malformation. Potential confounding factors include demographic characteristics, accompanying medications, comorbidities, and healthcare utilization measures.
Additionally, numerous sensitivity analyses were performed to assess the robustness of the findings. These included restricting the reference group to cephalexin or amoxicillin and restricting the cohort to symptomatic UTI using the definition of alternative outcomes. The team also investigated the pregnancy timing effect by narrowing the exposure window during critical organ development periods (e.g., 4-9 weeks for cardiac defects). Finally, the team examined the association between antibiotics and risk of cardiac malformations and malformations in a larger cohort of pregnant individuals who received UTI-related antibiotics for any indication.
Survey results
This study included 71,604 pregnancies, 59.2% were exposed to nitrophantin, 30.8% were exposed to β-lactam, 5.1% were exposed to fluoroquinolone, and 4.9% were exposed to TMP-SMX for UTI treatment during the first gestational period. Median gestational age at antibiotic exposure was significantly different. TMP-SMX and fluoroquinolone were prescribed earlier (26 days and after LMP, respectively) than β-lactam or nitrofluntine (63 days and 62 days). In total, 1,518 infants were identified with congenital malformations. The absolute, unmodulated risk of congenital malformations was 19.8, 21.2, 23.5, and 26.9 per 1,000 persons for β-lactam, nitrophantin, fluoroquinolone, and TMP-SMX. Estimates were similar for cardiac malformations.
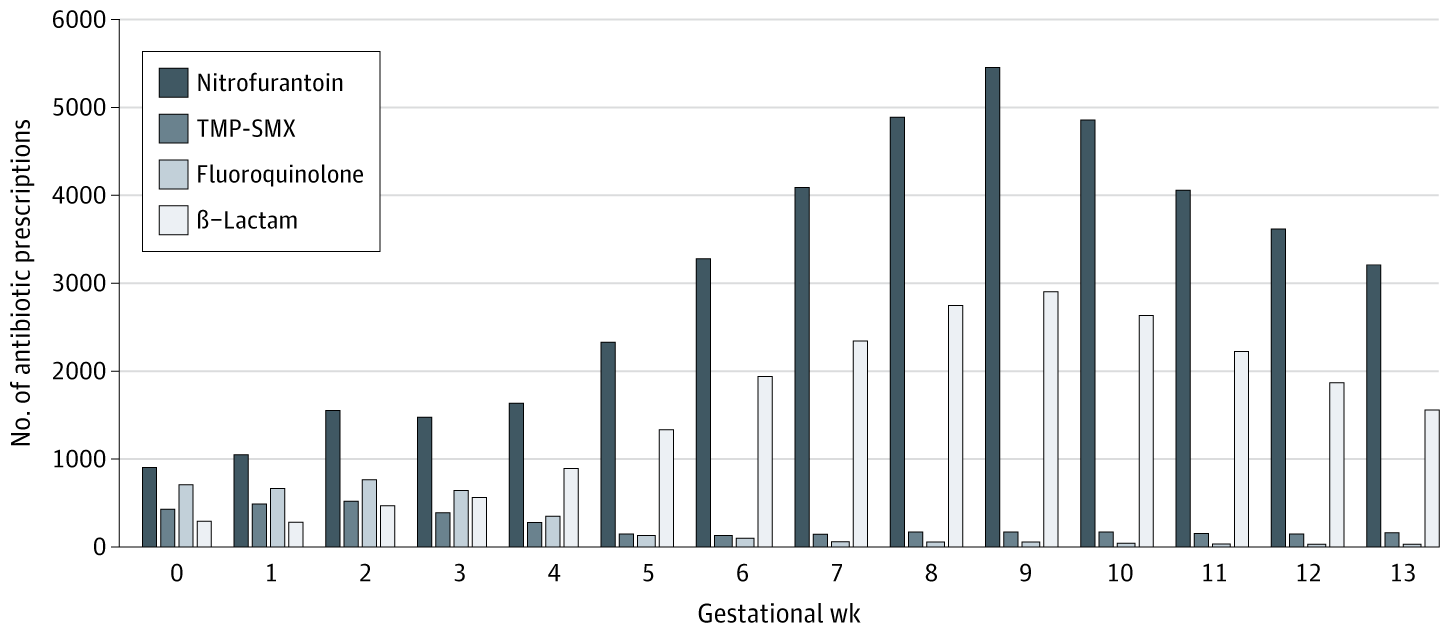 Median gestational age at the index of symptomatic UTI was 6 weeks (3-9) weeks compared to 9 (7-11) weeks of asymptomatic bacteriuria. TMP-SMX shows trimethoprim-sulfamethoxazole.
Median gestational age at the index of symptomatic UTI was 6 weeks (3-9) weeks compared to 9 (7-11) weeks of asymptomatic bacteriuria. TMP-SMX shows trimethoprim-sulfamethoxazole.
Infants exposed to TMP-SMX were at a higher risk of malformation compared to those exposed to β-lactam (adjusted RR 1.35; 95% CI 1.04-1.75). The researchers estimated that one additional malformation occurs for every 145 pregnancies exposed to TMP-SMX. The risk of malformation was similar for infants exposed to fluoroquinolone or nitrofurantoin compared to those exposed to β-lactams.
In organ-specific malformation analysis, the risk of cardiac malformation in β-lactam and TMP-SMX exposure pregnancy was similar, but TMP-SMX was associated with an increased relative risk of oral/respiratory malformation (RR 2.89; 95% CI 1.31-6.41), and specifically for severe Cardiact Depects, rr 2.09) (RR 1.52), and lip/palate (RR 3.23). However, these specific malformation risk difference estimates include null values, indicating absolute risk uncertainty.
Sensitivity analysis:
The definition of alternative outcomes and reference groups resulted in consistent results. Limiting to symptomatic UTIS (excluding ASB) did not significantly alter the estimate of effect. Analysis taking into account pregnancy timing showed that TMP-SMX risk persisted, but increased accuracy when narrowed to the organogenesis window.
Finally, the large cohort included 256,686 pregnant individuals who received UTI antibiotics for any indication. This alternative analysis was specifically designed to address potential confounding due to indications. In this cohort, the risk of malformation was higher among pregnancies that were specifically exposed to TMP-SMX due to UTI than in other indications. The risk was not altered by signs of other antibiotics. Furthermore, compared to those exposed to β-lactam, infants exposed to fluoroquinolone, TMP-SMX, or nitrofluntine had similar risks for cardiac malformations or malformations. However, fluoroquinolone analysis resulted in smaller sample sizes (n = 3,663), resulting in wider confidence intervals and more accurate estimates.
Conclusion
Together, TMP-SMX exposure for UTI treatment during the first gestation period was associated with a higher risk of congenital malformations. It was also associated with an increased relative risk (uncertain absolute risk) of severe heart, cleft lip, cleft palate, and other cardiac malformations compared to β-lactams.
In particular, nitrofurantoin had less risk of malformation compared to β-lactam. Although the findings were consistent across sensitivity analyses, fluoroquinolone comparisons should be interpreted with caution due to limited statistical power.
Limitations of this study include non-randomised design. This could expose results to residual confounding, possible outcome misclassification, exposure misclassification, selection bias due to restrictions on births, and the likelihood of disgenerabilization of outcomes to uninsured or Medicaid-insured populations.
Overall, the results support current recommendations for caution when using TMP-SMX during initial gestational periods, but do not support limits on the use of nitrofluntin.