Summary: Social isolation has a direct causal impact on how quickly cognitive function declines in old age, regardless of whether someone feels lonely. Analyzing more than 137,000 cognitive tests from more than 30,000 older adults, the study found that reduced social contact consistently predicted faster decline across all demographic groups.
Loneliness and isolation influence health, but only isolation reliably causes cognitive decline. With Alzheimer’s rates already high and no cure available, the findings highlight that strengthening social connection is not only emotionally beneficial but also neurologically protective.
Key facts:
Isolation as a cause: Objective social isolation (not just loneliness) directly accelerates cognitive decline. Consistent across groups: The effect appeared across levels of gender, race, ethnicity, and education. Large-scale evidence: Findings were based on more than 137,000 cognitive assessments collected over 14 years.
Source: University of St. Andrews
New research from the University of St Andrews has discovered a direct causal effect between social isolation and a more rapid decline in cognitive function in old age. Pathological cognitive impairment is usually caused by Alzheimer’s and related dementias
The study, published today (December 16, 2025) in The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, found a consistent pattern of greater social isolation causing faster cognitive decline, whether people identify as lonely or not.
Social isolation is measured objectively, such as sociability, membership in community organizations, and religious participation, while loneliness is a subjective report of how often people feel lonely.
Although social isolation and loneliness are often thought to be associated, they appear to have independent effects on cognitive function.
St Andrews’ School of Geography and Sustainable Development, together with researchers from the Max Planck Institute for Demographic Research in Germany and Emory University in the United States, analyzed data from the US Health and Retirement study, analyzing 137,653 cognitive function tests taken between 2004 and 2018 by more than 30,000 people.
They found that reducing social isolation has a protective effect on cognitive function in all subpopulations, regardless of gender, race, ethnicity, and educational level, with only minor differences between social categories.
There has been great interest in the health effects of social isolation and loneliness, especially in adolescents and older adults. Before Covid 19, around a quarter of older people (aged 65 and over) identified as socially isolated, raising concerns about the health implications. Likewise, loneliness has been recognized as a major public health problem in high-income countries, including the United States, the United Kingdom, Sweden, Australia, Germany, and Japan.
In the US, Alzheimer’s disease already affects around 6.9 million people, and around 1 in 11 people over the age of 65 suffer from it in the UK. With no known cure, prevention is very important.
Lead author of the paper, Dr Jo Hale from the University of St Andrews, said: “During the holidays, many of us think a lot about how important it is to be surrounded by family and friends. From pagan winter holidays to classic Christmas stories, we are reminded that social engagement is good for our mental health.
“This research shows that it is also important for our cognitive health. Given that Alzheimer’s is a leading cause of death among older adults in the UK and US, building the scaffolding to enable regular social interaction, especially for those who do not have family or friends nearby, should be a public health priority.”
Key questions answered:
A: The study shows a direct causal link: greater isolation predicts faster decline independently of subjective loneliness.
A: No. Loneliness is subjective and emotional, while isolation is behavioral; only isolation reliably boosted cognitive decline.
A: All subgroups studied (across all demographic lines) showed cognitive protection when isolation was reduced.
Editorial notes:
This article was edited by a Neuroscience News editor. Magazine article reviewed in its entirety. Additional context added by our staff.
About this research news on social isolation and cognition.
Author: Ruth Sanderson
Source: University of St Andrews
Contact: Ruth Sanderson – University of St Andrews
Image: Image is credited to Neuroscience News.
Original research: Open access.
“Disentangling social isolation, loneliness, and late-life function among older adults in the United States: Evidence from causal inference modeling” by Jo Hale et al. Series B gerontology journals
Abstract
Disentangling social isolation, loneliness, and later-life function among older adults in the United States: Evidence from causal inference models.
Goals
Older adults are at high risk for the negative health impacts of social isolation and loneliness. One of those potential negative health impacts is Alzheimer’s disease, a leading cause of death among adults in the United States and many high-income countries.
Taking a life course perspective, we explore whether there is a direct causal effect of social isolation on trajectories of cognitive function in later life, the extent to which any effect of social isolation on cognitive decline operates indirectly through loneliness, who may be most vulnerable, and the potential effectiveness of a statistical intervention for those living alone.
Methods
We used a counterfactual approach, the g formula, with the US Health and Retirement Study, which analyzes data from 30,421 people with 137,653 observations between 2004 and 2018.
Results
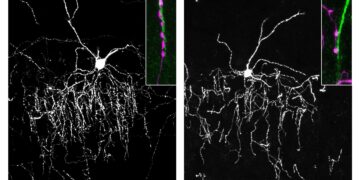
We found a consistent pattern of social isolation having a detrimental direct causal effect on cognitive function, with only 6% of this effect operating through loneliness. Reducing social isolation has a protective effect on cognitive function in all subpopulations, regardless of gender, race/ethnicity, and educational level, with only minor differences between social categories.
Our statistical intervention shows that addressing social isolation of those living alone may be a viable public health strategy to protect against cognitive decline.
Discussion
Our results suggest that addressing social isolation (and, by extension, its health effects) requires both a broad understanding of its heterogeneous impacts in the general population and a nuanced approach to targeting public health interventions where they can be most effective.