Summary: Scientists tested a multi-step immune therapy designed to retrain the body to control HIV without ongoing antiviral treatment. After stopping standard HIV medications, seven out of ten participants maintained low viral levels for prolonged periods and one showed no viral rebound at all.
The therapy worked by stimulating powerful virus-targeting T cells while reducing viral reservoirs with antibodies. The findings provide rare evidence that long-term HIV control can be achieved without drugs and could reshape future cure strategies.
Key facts
Sustained control: 70% of participants maintained low HIV levels after stopping daily medication. Immune reprogramming: A vaccine plus antibody therapy trained immune cells to suppress the virus. Delayed rebound: Only three participants showed the rapid viral return typically seen after stopping treatment.
Source: UCSF
A new study from the University of California, San Francisco shows that it is possible to control HIV without long-term antiviral treatment, a breakthrough that points the way toward a possible cure for a disease that affects 40 million people worldwide.
Treatment with a combination of experimental immunotherapy agents allowed seven out of 10 participants to keep the virus at low levels for many months after stopping antiretroviral therapy (ART).
The results appear on December 1, World AIDS Day, in Nature.
The trial, which was based on collaboration with nearly a dozen pharmaceutical companies and other partners in HIV research, offers proof of concept that the approach could work. Although the study was small and did not include a control group, researchers said the results are extremely encouraging.
“The majority had some evidence of control, which we think is unprecedented,” said the paper’s co-senior author, Steven Deeks, MD, a professor of Medicine at UCSF who is in the Division of HIV, Infectious Diseases and Global Medicine at Zuckerberg General Hospital in San Francisco.
“I think we are finally making real progress toward developing a therapy that can allow people to live healthy lives without the need for lifelong medications.”
The trial was made possible by the Foundation for AIDS Research’s (amfAR) five-year, $20 million partnership with UCSF to advance AIDS cure research, launched in 2015. It was also supported by the National Institutes of Health (NIH).
Reprogram the body’s immune system.
Antiretroviral therapy (ART) was introduced in the 1990s and turned HIV infection from a death sentence to a chronic disease. But it is not a cure and the virus remains in the body ready to reawaken as soon as someone stops taking ART.
The study was designed to test whether a triple combination of immunotherapies could reprogram the body’s immune system to control the virus after stopping ART. Most participants had started ART soon after acquiring HIV, which helped preserve their immune response.
First, participants received a therapeutic vaccine to stimulate their T cells (a part of the immune system that attacks viruses) to go after latent HIV in their bodies. Then, they received a cocktail of antibodies to reduce the amount of HIV in the body. Finally, they were given another round of anti-HIV antibodies before stopping ART.
Typically, when a person with HIV stops taking anti-HIV medications, the virus begins to recover in about two weeks and then spikes. This time, only three of the 10 patients experienced the typical rapid rebound. Six maintained low levels of the virus for months and one did not rebound at all.
The lunging cat analogy
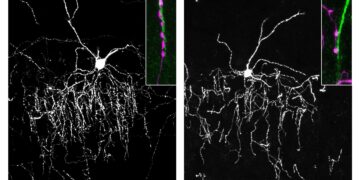
The researchers then examined the immune responses of those who controlled the virus to see how they did.
“It turns out that the drivers had T cells that were able to expand dramatically once they encountered the virus,” said Rachel Rutishauser, MD, PhD, associate professor in the UCSF Division of Experimental Medicine and co-senior author of the paper.
“It’s like they’re waiting for their target, kind of like a cat preparing to attack a mouse.”
The treatment would have to be simplified and proven effective in much larger studies before it could replace standard HIV treatment.
“This is not the end,” said Michael Peluso, MD, assistant professor in the UCSF Department of Medicine and first author of the study. “But it shows that we can drive progress on a challenge we often consider unsolvable.”
Authors: Other UCSF co-senior authors include Demi Sandel, PhD, Amelia Deitchman, PharmD, PhD, along with co-authors Steven Yukl, MD, Timothy Henrich, MD, Matthew Spitzer, PhD, David Glidden, PhD, Michiko Shimoda, PhD, Rebecca Hoh, Thomas Dalhusien, Hari Prabhath Tummala, PharmD, Sun Jin Kim, PhD, Gina Borgo, PhD, Rafael Tibúrcio, PhD, Lily Zemelko, Kaiti Schwartz, Monika Deswal, Meghan Williams, RN, and Mandana Khalili, MD.
Funding: The UCSF amfAR pooled trial was funded by amfAR: The Foundation for AIDS Research (109301-59-RGRL). The ATI prospective study was funded by the Bill & Melinda Gates Foundation (INV-002707). Additional support was provided by NIH (UM1AI164560), (K23AI157875), (K23AI162249), (R01AI170239), (P01AI178375), (P01AI16960), (T32GM136547), (T32AI060530), (K24AA022523), (R01DE032031008), (P30AI027763), (S101S10OD01804001), (P30AI152501), Cancer Research Institute award CR14437 and amfAR (110560-74-RPRL). This research was also supported in part by the NIH Intramural Research Program and the NIH National Center for Advancing Translational Sciences through the UCSF CTSI (UL1 TR001872).
Key questions answered:
A: In this small clinical trial, most participants maintained low levels of virus for months after stopping standard HIV medication.
A: A combination of therapeutic vaccination and targeted antibodies retrained the immune system to suppress the virus.
A: It is not yet a cure, but it provides strong evidence that long-term control without medications is possible.
Editorial notes:
This article was edited by a Neuroscience News editor. Magazine article reviewed in its entirety. Additional context added by our staff.
About this HIV and immunotherapy research news
Author: Laura Kurtzman
Source: UCSF
Contact: Laura Kurtzman – UCSF
Image: Image is credited to Neuroscience News.
Original Research: Closed access.
“Correlates of HIV-1 control after combination immunotherapy” by Steven Deeks et al. Nature
Abstract
Correlates of HIV-1 control after combination immunotherapy
Identification of therapeutic strategies to induce sustained control of HIV infection without antiretroviral therapy (ART) is an important priority.
Combination immunotherapy, including HIV vaccination, immune stimulation/latency reversal, and passive transfer of broadly neutralizing antibodies (bNAbs), has shown promise in non-human primate models, but few studies have translated these approaches to people.
We conducted a single-arm proof-of-concept study in ten HIV-infected individuals receiving ART combining the following three approaches: (1) therapeutic vaccination with a DNA+IL-12/MVA booster regimen targeting the conserved element (CE) of HIV/Gag followed by (2) administration of two bNAbs (10-1074, VRC07-523LS) and a toll-like receptor 9 agonist (lefitolimod) during withdrawal. ART, followed by (3) repeat bNAb administration at the time of ART discontinuation (NCT04357821).
Seven of the ten participants showed postintervention control after stopping ART, regardless of residual plasma bNAb levels. The strong early expansion of activated CD8 + T cells in response to virus rebound correlated with a lower mean viral load after peak viremia without ART.
These data suggest that combination immunotherapy approaches could be effective in inducing sustained HIV control by delaying rebound and enhancing CD8+ T cell responses, and that these approaches should continue to be optimized.