Summary: Researchers developed an artificial intelligence tool that detects chronic stress by measuring adrenal gland volume in routine chest CT scans. This biomarker aligns with cortisol levels, stress questionnaires, and future cardiovascular outcomes, offering the first image-based method to quantify stress load on the body.
The findings show that greater adrenal volume is related to greater stress, greater allostatic load, and greater risk of heart failure and mortality. With millions of CT scans already performed each year, this approach could transform the early detection and prevention of stress without requiring new tests or radiation.
Key facts
AI Stress Biomarker: Adrenal gland volume measured from CT scans reflects long-term chronic stress more reliably than momentary cortisol tests. Risk Prediction: Greater adrenal volume is associated with elevated cortisol, greater allostatic load, and increased risk of future heart failure. Clinical Potential: This biomarker can be extracted from routine imaging and offers a scalable tool for early prevention of stress-related diseases.
Source: RSNA
Using a deep learning artificial intelligence model, researchers have identified the first chronic stress biomarker detectable through routine imaging, according to research to be presented next week at the annual meeting of the Radiological Society of North America (RSNA).
Chronic stress can affect physical and psychological well-being, causing a variety of problems including anxiety, insomnia, muscle pain, high blood pressure and a weakened immune system, according to the American Psychological Association. Research shows that chronic stress can contribute to the development of serious diseases, such as heart disease, depression and obesity.
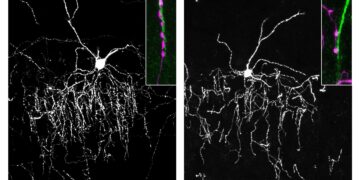
The study’s lead author, Elena Ghotbi, MD, a postdoctoral researcher at Johns Hopkins University School of Medicine in Baltimore, Maryland, developed and trained a deep learning model to measure adrenal gland volume on existing CT scans.
Tens of millions of chest CT scans are performed each year in the United States alone.
“Our approach leverages widely available imaging data and opens the door to large-scale assessments of the biological impact of chronic stress on a variety of conditions using existing chest CT scans,” Dr. Ghotbi said.
“This AI-driven biomarker has the potential to improve cardiovascular risk stratification and guide preventive care without additional testing or radiation.”
Lead author Shadpour Demehri, MD, professor of radiology at Johns Hopkins, said chronic stress is a common condition or complaint that many adults face daily.
“For the first time, we can ‘see’ the long-term burden of stress within the body, using a scan that patients already have every day in hospitals across the country. Until now, we have not had a way to measure and quantify the cumulative effects of chronic stress, other than questionnaires, surrogate serum markers such as chronic inflammation, and measurement of cortisol, which is very cumbersome to obtain.” Dr. Demehri said.
Unlike single measurements of cortisol, which provide a momentary snapshot of stress levels, adrenal volume acts as a biological barometer of chronic stress.
In the study, researchers obtained data on 2,842 participants (mean age 69.3; 51% women) from the Multi-Ethnic Study of Atherosclerosis, a comprehensive study that combines chest CT scans, validated stress questionnaires, measures of cortisol, and markers of allostatic load—the cumulative physiological and psychological effects of chronic stress on the body. This rare integration of imaging, biochemical, and psychosocial data made it the optimal, and likely only, cohort to develop an imaging biomarker of chronic stress.
The researchers retrospectively applied their deep learning model to CT scans to segment and calculate the volume of the adrenal glands. Adrenal volume index (AVI) was defined as volume (cm³) divided by height² (m²). Salivary cortisol was collected eight times a day for two days. Allostatic load was based on body mass index, creatinine, hemoglobin, albumin, glucose, white blood cell count, heart rate, and blood pressure.
Statistical associations between AVI and cortisol, allostatic load, and measures of psychosocial stress, including depression and perceived stress questionnaires, were evaluated. The researchers found that AI-derived AVI correlated with validated stress questionnaires, circulating cortisol levels, and future adverse cardiovascular outcomes.
Higher AVI was associated with higher cortisol, peak cortisol, and allostatic load. Participants with high perceived stress had higher AVI compared to those with low stress. AVI was also associated with a higher left ventricular mass index. Every 1 cm³/m² increase in AVI was associated with an increased risk of heart failure and mortality.
“With up to 10 years of follow-up data from our participants, we were able to correlate AI-derived AVI with clinically meaningful and relevant outcomes,” Dr. Ghotbi said.
“This is the first chronic stress imaging marker that has been validated and shown to have an independent impact on a cardiovascular outcome, namely heart failure.”
“For more than three decades, we have known that chronic stress can wear down the body in multiple systems,” said Teresa E. Seeman, Ph.D., co-author of the study and professor of epidemiology at UCLA and a pioneering researcher in stress and health.
“What makes this work so exciting is that it links a routinely obtained imaging feature, adrenal volume, to validated biological and psychological measures of stress and shows that it independently predicts an important clinical outcome. It is a real step forward in operationalizing the cumulative impact of stress on health.”
Dr. Demehri said that by linking an easily measurable imaging feature to multiple validated indicators of stress and subsequent illness, this research introduces an entirely new practical way to quantify chronic stress.
“The key importance of this work is that this biomarker can be obtained from CT scans that are widely performed in the United States for a variety of reasons,” Dr. Demehri said. “Second, it is a physiologically sound measure of adrenal volume, which is part of the physiological cascade of chronic stress.”
The researchers said the imaging biomarker could be used in a variety of diseases associated with chronic stress in middle-aged and older adults.
Other co-authors are Roham Hadidchi, Seyedhouman Seyedekrami, Quincy A. Hathaway, MD, Ph.D., Michael Bancks, Nikhil Subhas, Matthew J. Budoff, MD, David A. Bluemke, MD, Ph.D., R. Graham Barr, and Joao A.C. Lima, MD
Key questions answered:
A: They identified the first image-based biomarker of chronic stress using adrenal gland volume measured by AI.
A: It reflects long-term physiological stress, correlating with cortisol, allostatic load and future cardiovascular risk.
A: Cortisol fluctuates throughout the day; Adrenal volume provides a stable, cumulative indicator of long-term stress load.
Editorial notes:
This article was edited by a Neuroscience News editor. Magazine article reviewed in its entirety. Additional context added by our staff.
About this news on stress and AI research
Author: Linda Brooks
Source: RSNA
Contact: Linda Brooks – RSNA
Image: Image is credited to Neuroscience News.
Original research: Findings will be presented at the 111th Scientific Assembly and Annual Meeting of the Radiological Society of North America (RSNA).