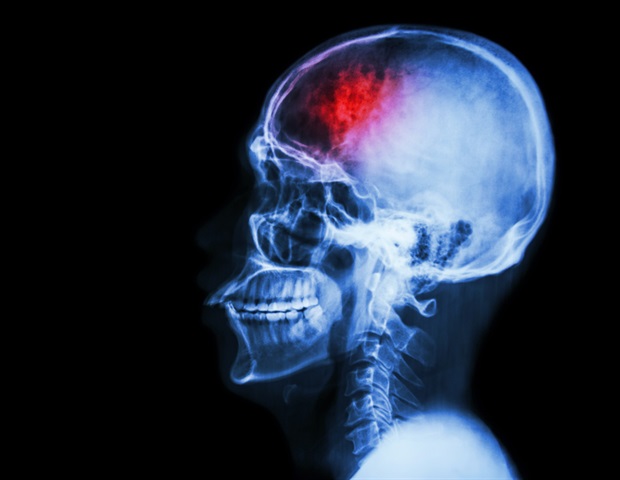
Summary: New international studies reveal that schizophrenia appears differently in the brain, reflecting a wide range of symptoms in patients. Researchers analyzed image data from more than 6,000 individuals and found that while some brain structures differed significantly, others remained very uniform.
Brain folding patterns in the midfrontal region are consistently similar across patients, suggesting a less flexible developmental process in childhood. These findings highlight the need for a precision medical approach tailored to each patient’s neurobiological profile.
Important facts
Brain Structure Variability: Schizophrenia patients show significant differences in brain surface area and thickness. Mind-to-developmental properties: Consistent brain folding in the mid-frontal region suggests early developmental rigidity in schizophrenia.
Source: University of Zurich
Symptoms of schizophrenia vary widely from person to person. New research shows how these differences manifest themselves in brain structure.
Schizophrenia is a complex mental health condition that affects perception, thoughts and emotions. This complexity is reflected in the individual symptoms of the disease. For some patients, perceptual disorders are the main problem, while for others, cognitive disorders are more common.
“In this sense, there are not just one schizophrenia, but many people have different neurobiological profiles,” says Wolfgang Omlor, the first author of the study and a senior physician at the University of Psychiatry Hospital.
To do justice for each of these types of schizophrenia, precision medicine approaches must be adopted, such as treatments that are accurately consistent with their respective neurobiological profiles.
“This requires an approach that seeks both individual differences and similarities at the neurobiological level,” explains Omler.
Comprehensive international study of patient brain structure
In an international multicenter study, researchers from Wolfgang Omler and the University of Zurich examined the variability of brain structures in patients with schizophrenia.
The researchers have examined several properties, including the thickness and surface area of the brain cortex, and the folding patterns and volume of deeper brain regions.
The data was obtained from Enigma Collaboration, an international research project that combines image data from over 6,000 people from 22 countries. By comparing the brain structures of thousands of patients, schizophrenia and healthy individuals, the variability of brain structures can be studied with high reliability.
The development of the brain with low flexibility in childhood has been revealed
Although the brain structure of schizophrenia varies, it may reflect differences in symptoms between patients, the uniformity of the brain folding in the brain frontal brain region suggests developmental properties common to people with schizophrenia.
Because brain folding is largely completed in childhood, brain development during this period appears to be inflexible in schizophrenia patients, especially in areas that link thought and emotional processes.
“These findings broaden our understanding of the neurobiological foundations of schizophrenia,” says the Phillip Homann professor at the University of Zurich and the corresponding author of the study.
“While uniform brain folding may indicate a possible mechanism for disease development, regions with a high degree of variability in brain structures may be associated with the development of individualized therapeutic strategies.”
About this schizophrenia research news
Author: Barbara Simpson
Source: University of Zurich
Contact: Barbara Simpson – University of Zurich
Image: Image credited to Neuroscience News
Original research: Open access.
“Estimation of multimodal structural brain variability in schizophrenia spectrum disorders: A study of global mysteries,” Philipp Homan et al. American Journal of Psychiatry
Abstract
Estimation of multimodal structural brain variability in schizophrenia spectral disorders: a global enigma study
Objective:
The authors synthesized evidence from studies quantifying the relationship between anticholinergic drugs and cognitive function in psychosis, and further investigated studies examining whether reducing anticholinergic drugs affects cognitive functioning in psychotic individuals.
method:
Database searches were conducted at Medline, Emmaze, and PsyCINFO from database inception until October 2023 for studies reporting objective cognitive assessment and quantification of anticholinergic load using clinical scale, serological anticholinergic activity, or tapering of anticholinergic therapy. Analysis was performed in R using the Metafor package. A meta-analytical model of random effects was employed, and assessments of heterogeneity, study quality, and meta-regression (age, gender, and antipsychotic dosage in chlorpromazine equivalents) were employed.
result:
Of the 1,337 citations, 40 inclusion criteria consisting of 25 anticholinergic load studies (4,620 patients), 6 serological anticholinergic activity studies (382 patients), and 9 tapering studies (186 patients). A negative correlation was identified between anticholinergic loading and global cognition (r = -0.37, 95% CI = -0.48, -0.25), verbal learning (r = -0.28, 95% CI = -0.36, -0.21), and visual learning (R = -0.17, 95% CI = 95% CI = 95% CI = 95% CI = 95% CI = -0.36, -0.21). -0.06), working memory (r = -0.22, 95% CI = -0.29, -0.14), processing speed (r = -0.24, 95% CI = -0.35, -0.13), caution (r = -0.19, 95% CI = -0.29, -0.08). (r=-0.17, 95% CI=-0.27, -0.06), and social cognition (r=-0.12, 95% CI=-0.19, -0.05), and between serological anticholinergic activity and language learning (r=-0.0.14, 95% CI=-0.38, (r=-0.19, 95% CI=-0.35, -0.03), and executive function (r=-0.16, 95% CI=-0.27, -0.04). Finally, with the removal of anticholinergic drug therapy, oral learning (d=0.77, 95% CI=0.44, 1.1), working memory (d=0.94, 95% CI=-0.94, 95% CI=-0.04). Finally, with the removal of anticholinergic drug therapy, oral learning (d=0.77, 95% CI=0.44, 1.1), working memory (d=0.94, 95% CI= 0.63, 1.26) and for executive function (d = 0.44, 95% CI = 0.26, 0.62).
Conclusion:
Anticholine burden is associated with cognitive impairments observed in psychosis. From a clinical perspective, tapering anticholinergic drugs in psychotic patients can improve cognition. However, randomized clinical trials are required for fair quantification of benefits.