A collaboration between civil engineering and neurosurgery at the University of Pittsburgh could change the way spinal fusion surgery is performed and monitored. Associate Professors Amir Alavi, Nitin Agarwal, and D. Kojo Hamilton received a $352,213 National Institutes of Health (NIH) R21 grant to develop the first self-powered spinal implant capable of transmitting real-time data from inside the body.
The transdisciplinary project, “Wireless Metamaterial Interbody Cage for Real-Time Evaluation of Lumbar Spinal Fusion in Vivo,” could make spinal fusion recovery safer by allowing doctors to track progress remotely and intervene before complications arise.
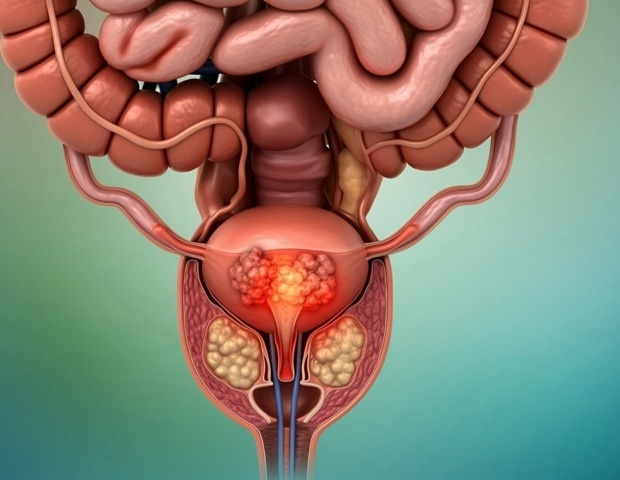
Each year, up to one million Americans undergo spinal fusion surgery, which uses a metal cage and bone graft to fuse two vertebrae in the spine, with screws and brackets holding these bones in place.
“After the hardware is implanted, we monitor it using “This means patients have to make in-person visits and undergo radiation.”
Because doctors and patients can’t easily monitor the spine as it heals, it’s not a connected healthcare experience, explained Agarwal, who also directs Minimally Invasive Spine and Robotic Surgery at UPMC.
While implantable wireless devices that monitor medical procedures are becoming more common and could help alleviate these problems, the devices require batteries and an electronic component to transmit signals, making them non-permanent.
Alavi, principal investigator and associate professor and BP America faculty member in the Department of Civil and Environmental Engineering, turned to an unexpected place for a better solution: the technology he helped develop to monitor bridge infrastructure.
As a doctoral student, Alavi created sensors that produce their own energy and send signals that indicate changes in the physical properties of the bridges. These sensors alert officials to structural weaknesses before more serious damage develops. Alavi thought the technology could be adapted to work on a patient’s spine.
“No batteries, no antennas, no live electronics, don’t worry!” said Alavi, who also heads the Intelligent Structures and Architectural Materials Research and Testing Laboratory (ISMART). “By combining metamaterial design with nanoenergy harvesting, we create completely battery-free implants and electronic devices that power themselves through contact electrification. They adapt to each patient and transmit signals wirelessly like a mini router inside the body.”
Using new human-developed compounds known as metamaterials, Alavi’s team has created structures consisting of unit cells of different sizes. By interweaving conductive and non-conductive materials, they can optimize these structures to harvest energy and transmit signals when pressure is applied.
From bridges to the back
In 2023, Alavi and Agarwal began a seemingly unlikely collaboration that integrated this technology into medical implants. The promise of their research is described in the Materials Today article “Wireless Mechanical Metamaterial Implants Without Electronics.”
“We are creating cages for spinal fusion surgery that, like human cells, have natural intelligence built into them.”
Amir Alavi, associate professor, University of Pittsburgh
These cages are placed between two vertebrae and provide stability while monitoring the healing process.
“If the spine is healing, the bone begins to bear more load and the signal self-generated by the implant naturally decreases,” Alavi noted. “Immediately after surgery, the signal is stronger because the vertebral plates press harder on the cage, so it generates more energy.”
Signals are received through an electrode on the patient’s back and transmitted to the cloud, where they can be interpreted in real time, allowing medical intervention before more serious damage occurs.
Alavi also turned to generative AI to generate unique metamaterial designs for each patient’s spine, dramatically speeding up the process.
“We can scan the patient’s spine and then design and print the cage to fit perfectly. There are different types of patient-specific porous cages on the market, but ours is a metamaterial system with full control over stiffness and, more importantly, the ability to generate its own energy, which we use not only for monitoring, but are now working to apply electrical stimulation as well.”
Alavi and Agarwal have tested in vitro cages and the technology works. With support from the NIH, the team will conduct in vivo testing using animal models. “If it works,” Agarwal said, “then the next step will be human testing.”
He added: “By combining clinical and laboratory expertise, we have a better chance of translating science into patient use, improving safety and outcomes, while creating more connected healthcare.”


_6e98296023b34dfabc133638c1ef5d32-620x480.jpg)