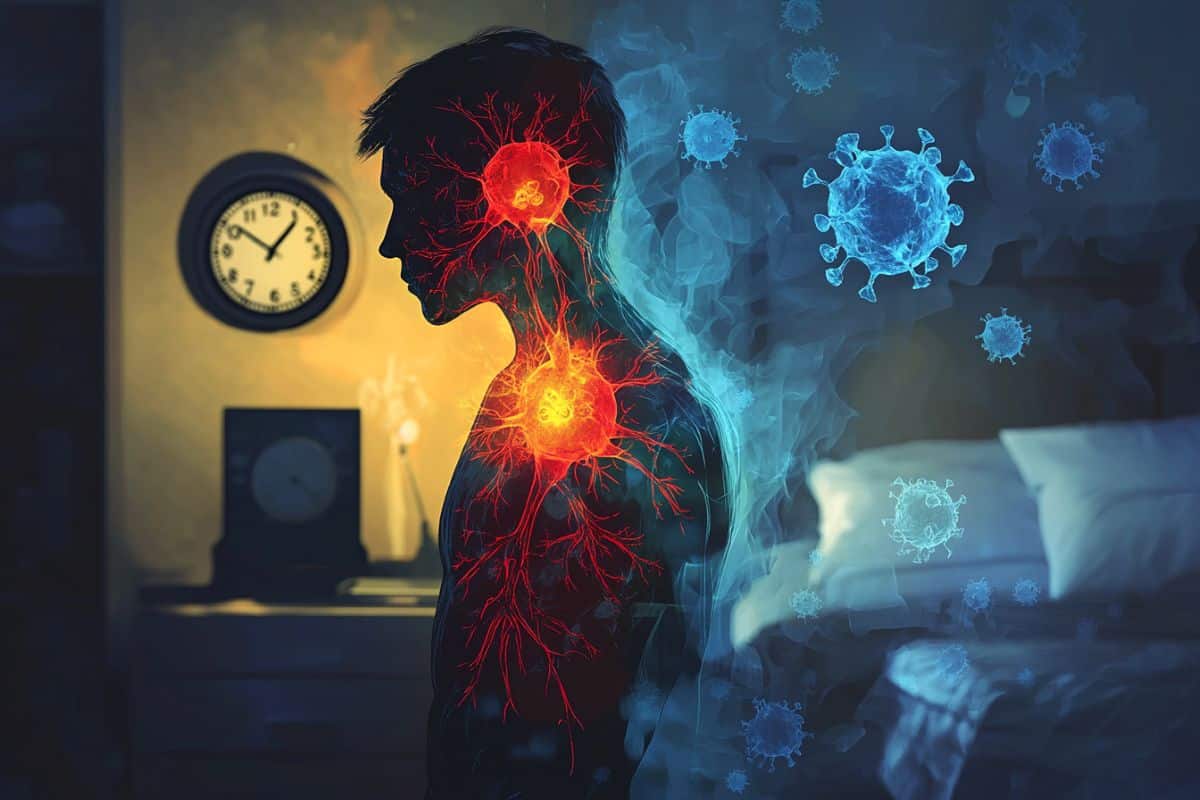
Summary: A new study reveals that even one night of sleep deprivation changes the profile of immune cells, resembling what is seen in obesity, and conditions associated with chronic inflammation. The researchers found that sleep-deprived individuals had increased levels of nonclassical monocytes in immune cells associated with inflammatory responses, similar to the patterns observed in obese participants.
These findings suggest that poor sleep quality can cause rapid changes in the immune system and may potentially contribute to long-term inflammatory diseases such as obesity, diabetes and cardiovascular disease. I’m doing it. Future research will investigate whether interventions like structured sleep therapy can reverse these immune changes and improve overall health.
Important facts
Sleep and Immune Health: A sleep-deprived night alters immune cells and mimics the inflammation patterns seen in obesity. It can contribute to inflammation-driven conditions such as obesity, diabetes, and heart disease.
Source: AAI
New research reveals insights into how sleep quality affects a person’s immune system and how it relates to the development of diseases such as obesity, diabetes and cardiovascular disease.
This study, published in the Journal of Immunology, shows that even a 24-hour sleep-deprived night in young, lean, healthy individuals, immune cell profiles that help regulate the immune system are profiled in obese individuals. I found out that I could change it. A condition known to promote chronic inflammation.
This suggests that the immune system is extremely sensitive to sleep and may rapidly adapt to changes in sleep patterns. Researchers say that if these shifts persist, they can contribute to long-term inflammatory conditions and increase the risk of disease.
There is substantial evidence linking sleep disorders and disorders to a range of chronic conditions and morbidity, including type 2 diabetes and cardiovascular disease. It is also known that low health outcomes can be driven by chronic inflammation, but the direct effects of sleep on circulating immune cells such as monocytes are not well understood.
Monocytes are an important component of the innate immune system. This is the body’s first line of defense that rapidly detects pathogens and kicks off an immune response. Monocytes come in three subsets: classical, intermediate and non-classical monocytes.
Non-classical monocytes help patrol the body, sense inflammatory cues, respond to, and maintain and regulate immune responses.
In this study, researchers from the Dasman Diabetes Institute in Kuwait, Kuwait, analyzed sleep patterns in 237 healthy adult participants with various BMIs, collected blood samples and obtained different monocyte levels. and markers of inflammation were profiled.
They found that obese individuals had significantly lower quality of sleep and higher chronic low-grade inflammation compared to the lean group.
Nonclassical monocytes were also significantly increased in obese participants, correlated with reduced sleep quality and increased proinflammatory markers.
Five healthy leans also participated in the 24-hour sleep deprivation section of the study, collecting blood samples throughout.
Researchers found that sleep deprivation alters monocyte profiles like those seen in obese participants, supporting the role of sleep health in regulating inflammation.
Dr. Fatema Al Rash, who led the study, said: Technological advances, long-term screen times, and changes in social norms become increasingly destructive to normal sleep duration.
“This sleep disruption has a major impact on immune health and overall well-being.”
Next, researchers want to explore in greater detail the mechanisms that link sleep deficiency to changes in immune system. They also want to investigate whether interventions such as structured sleep therapy and technical application guidelines can reverse these immunity changes.
“In the long term, this study aims to drive policies and strategies that recognize the important role of sleep in public health. We are particularly concerned with the risk of sleep disruption due to technical and professional demands. It envisions workplace reform and education campaigns that promote better sleep practices for a population.
“Ultimately, this could help reduce the burden of inflammatory diseases such as obesity, diabetes and cardiovascular disease,” said Dr. Allash.
About this sleep and inflammation research news
Author: Matt Lamb
Source: AAI
Contact: Matt Lam – Aai
Image: Image credited to Neuroscience News
Original research: Open access.
Fatema al-Rashed et al. Journal of Immunology
Abstract
The effect of sleep deficiency on monocyte subclasses and function.
The relationship between lack of sleep, obesity, and systemic inflammation is an important area of research as it has a significant impact on health. It has been established that lack of sleep has a negative effect on obesity and metabolic syndrome, but certain mechanisms, particularly asymptomatic inflammation, remain unknown, independent of obesity.
This study investigates how sleep quality affects monocyte subclass distribution and how the association with systemic inflammation affects the distribution of monocytes across various body mass index categories.
In our cohort study, 237 healthy participants were classified by body mass index. Participants’ dietary intake, physical activity, and sleep patterns were objectively tracked via a wearable actigraph GT3X accelerometer.
Data showed that obese individuals had significantly lower sleep quality and had higher chronic low-grade inflammation. Nonclassical monocytes are significantly increased in obesity, correlated with poor sleep quality and elevated proinflammatory cytokines.
Although the body mass index emerged as an important factor in promoting inflammation, mediation analysis further defined sleep disruption independently contributes to inflammation regardless of obesity status.
Controlled sleep deprivation experiments confirmed these findings, indicating a reversible increase in the expression of nonclassical monocytes.
This study highlights the importance of sleep quality in regulating immune responses and inflammation in obesity, suggesting that improving sleep quality reduces inflammation and improves health outcomes I’m doing it.